Nearly 5.5 million people in Canada will experience depression during their lives. Of those, 1.6 million will find no relief from conventional treatments.
Difficult-to-treat depression requires new options and dedicated research to give patients a path to reclaim their lives.
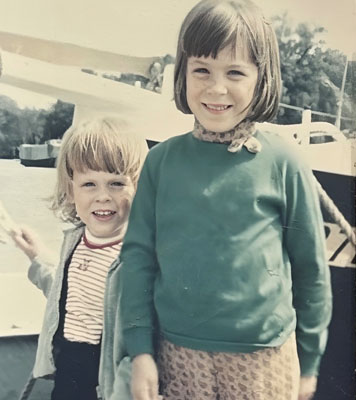
Marion Beckett knows how important it is to access new treatments for mental illness. A former nurse, Marion has lived with depression her entire life. “My mental health story started a long, long, long time ago,” she recalls.
Both of her parents suffered from mental illness—her father was not diagnosed until after his retirement and her mother was never officially diagnosed.
Marion wasn’t officially diagnosed until her early 30s. At that time, she was working as a cardiac nurse at an Ottawa hospital. Job-related stress added to personal struggles and eventually, led to a breakdown for which she was hospitalized.
It took two years to find a medication that worked. Marion looks back at that dark time and calls it desperate and exhausting.
Balance is essential but challenging
Side effects of medications to treat depression are very common. Some of these unwanted reactions include weight gain, insomnia, nausea or fatigue, all of which can have a negative impact on one’s quality of life alongside depression. A challenge of mental illness treatment is finding a medication that works and has minimal side effects.
Marion and her care team eventually found a medication that struck the right balance.
“It was not a silver bullet by any stretch of the imagination, but I felt better than I did before, and I was okay,” Marion describes. “I was good with that. I was much more functional.”
With medication and therapy, she “held steady” until a second mental health crisis in early 2019. A series of tragedies in her personal life led to another hospitalization. The Royal was the only hospital in the region that could offer her a lifeline. It was a harrowing time.
“It took a month just to patch me back together,” Marion says. But her treatment didn’t end there. Her care team saw Marion as someone who could greatly benefit from a research project inside the organization.
This time Marion was offered the opportunity to take part in a clinical study that involved ketamine—widely used as an anesthetic for decades. Recently, thanks to pioneering research from The Royal, it has emerged as an effective treatment for depression.

A potential breakthrough from Royal research
Esketamine, administered as a nasal spray under medical supervision, was approved by Health Canada in 2020. It targets specific pathways in the brain and increases the brain's ability to make new connections that can support recovery from depression. This can rapidly reduce depressive symptoms and thoughts of suicide in patients who have failed to respond to other commonly prescribed medications.
The Royal is a global leader in this area of research. The first clinical trials of ketamine as a treatment of depression in Canada were conducted at The Royal, with Dr. Pierre Blier, who had been studying ketamine’s effect on depression since 2010. The outcome of this work was published in 2019 in the American Journal of Psychiatry.
“The discovery of ketamine’s antidepressant effects has been hailed as one of the biggest breakthroughs in the field of depression in the past half-century,” says Dr. Jennifer Phillips, lead author and scientific director at The Royal.
“Research has shown us that esketamine is working for more patients with depression than conventional medications, and working much faster. So people who haven't responded to other treatments, sometimes for several years, might respond to this treatment,” says Phillips. “Esketamine is still new—we're translating it from clinical trials in a research setting into regular care. We want to know: Who does this work best for? How can we use this medication to maximize and prolong its effects? And how do we use it in association or conjunction with existing therapies that we might use for depression?”

Research helps patients faster
As a teaching and research hospital, The Royal can integrate research directly into patient care. This is a key element of the BMO Innovative Clinic for Depression, which offers novel treatments based on the latest science. Not only does this lead to better outcomes for patients, it creates an environment that helps researchers to answer some big questions around esketamine.
Marion’s treatment began in May 2022 and ended in January 2023. She says that while her other medications have kept her stable, she describes the addition of esketamine to her treatment plan as the missing piece of the puzzle.
“The way my brain processes things has absolutely changed,” Marion says.
She no longer thinks of herself as simply managing—she has her life back.
Marion hopes the establishment of the clinic inspires other donors and large organizations to lend their support to similar mental illness initiatives: “It really takes leadership to support a cause that has so much stigma around it,” Marion says.
On May 30, 2023, BMO announced a $2 million donation to establish the BMO Innovative Clinic for Depression at The Royal. This clinic offers new treatment options, develops research opportunities, and provides links to other treatments and services at The Royal.
It’s your turn to make an impact.
One in four Canadians live with mental illness or addiction, but only one in fifteen actually get effective treatment. The time for change is now—join us.