Eight innovative research projects funded through the annual University Medical Research Fund (UMRF) grant competition will harness Virtual Reality technology; EMRs; brain imaging and more, to improve diagnosis, treatment and prevention of mental illness, and promote access to care.
A therapy for schizophrenia that enables patients to better manage their auditory-visual hallucinations through the use of cutting-edge AVATAR technology.
Predictive models that will build on electronic medical records (EMRs) to accurately identify outpatients at greatest risk of suicide, through machine-learning.
A brain-based ‘marker’ that could quickly and objectively determine the right treatment path for individuals with post-traumatic stress disorder.
These are just a few of the innovative approaches to mental health care supported by the 2018-19 UMRF competition.
If they sound a bit futuristic – well, they are. But the future isn’t actually that far off.
Thanks to UMRF funding, the teams behind these (and other) forward-thinking research projects at The Royal will be supported as they embark on cutting-edge studies to improve care, and help people with mental illness get better, faster.
“Part of our vision of The Royal as a hospital without walls is focused on integrating research at points of care and removing any barriers that may stand in between clinical care and research; for the ultimate benefit of our patients,” says Dr. Joanne Bezzubetz, President & CEO of The Royal.
“By exploring and pushing the boundaries of our knowledge in a way that is integrated with care and driven by the needs and experiences of our patients, we can create better futures for all people living with mental illness.”
Congratulations to all of this year’s recipients!
The UMRF grant competition is made possible by contributions from the members of The Royal’s Associates in Psychiatry, and was established to foster cutting-edge, multi-disciplinary research at The Royal which closely integrates research and care, and has the potential to positively impact patient outcomes.
Avatar therapy for treatment of persistent auditory hallucinations in schizophrenia
(Funded $50,000; 1 year)
Research Team: Dr. Alexandra Baines (Principal Investigator), Dr. Nicola Wright (Co-Investigator), Ms. Nancy Bahi, Dr. Aaron Brinen, Dr. Clifford Cassidy, Dr. Faye Doell, Dr. Tom Fogl, Ms. Laura Friberg, Mr. Tyrone Gamble, Ms. Peggy Hickman, Dr. Martin Lepage, Dr. Mahesh Menon, Ms, Lisa Murata, Ms. Skylar Murphy Kelsey, Dr. Tim Ramsay, Ms. Carrie Robertson, Ms. Jessica Tutino
This international, multi-centre study will explore audio visual assisted therapy aid for refractory auditory hallucinations (AVATAR therapy) as a safe and effective therapy approach for those who hear voices. Using digital software, patients will work with therapists to create and interact with a visual representation of their voice, and learn new engagement and empowerment strategies. Given that auditory visual hallucinations are present in approximately 70% of individuals with schizophrenia – and about 25% of patients do not respond to anti-psychotics – new treatment approaches are critical to reduce distress and improve quality of life.
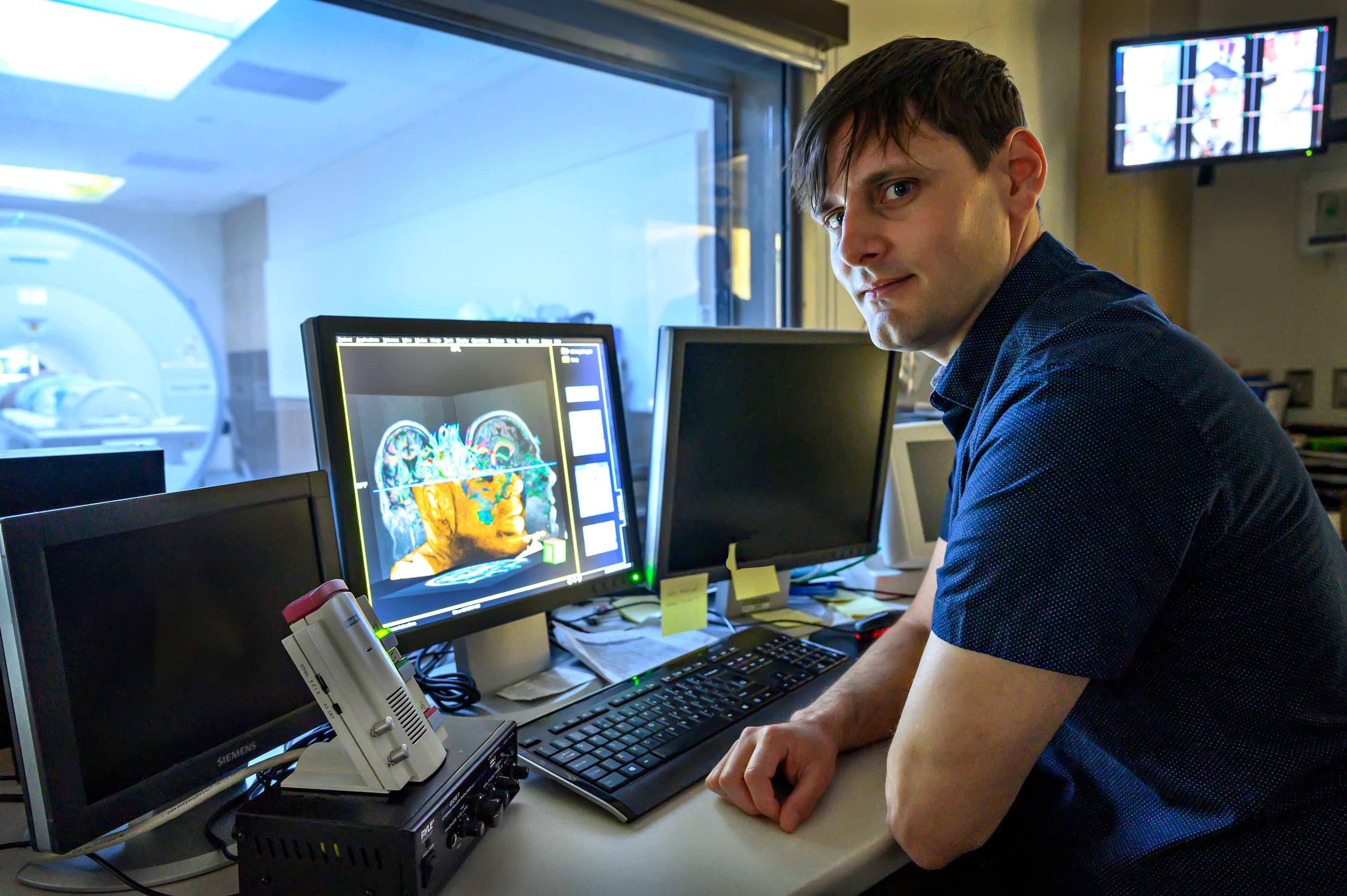
Neuromelanin-sensitive MRI as a marker of norepinephrine imbalance in PTSD
(Funded $50,000; 1 year)
Research Team: Dr. Clifford Cassidy (Principal Investigator), Dr. Rakesh Jetly, Dr. Jakov Shlik, Dr. Lauri Tuominen
This study will investigate the use of a ground-breaking new brain imaging technique (neuromelanin-sensitive MRI – or NM-MRI) as a novel biomarker for post-traumatic stress disorder (PTSD). This technique, recently validated as a biomarker for schizophrenia, could help to predict treatment response, and would allow for more directed treatment for those experiencing hyperarousal symptoms in PTSD (e.g. irritability; difficulties falling asleep or staying asleep; issues with concentration; impulsivity; anxiety; etc.). Project participants will include Canadian Armed Forces (CAF) members with a history of military-related trauma.
Predicting suicide attempt risk in psychiatric inpatients using electronic medical records and machine learning
(Funded $49,970; 1 year)
Research Team: Dr. Jennifer Phillips (Principal Investigator), Dr. Katerina Nikolitch, Dr. Robyn McQuaid, Dr. Zachary Kaminsky
This study will develop and validate algorithms to predict the risk of suicide attempts following psychiatric hospitalization using electronic medical records (EMRs) and machine learning, with the goal to inform more effective program and policy interventions for suicide prevention. The central hypothesis is that for individuals admitted to psychiatric facilities as a threat or danger to themselves, analysis of the data collected in EMRs during their inpatient stay could enable prediction of their suicide attempt risk following their discharge from hospital.
Metabolic correlates of antidepressant response to ketamine and electroconvulsive therapy: A pilot FDG-PET study
(Funded $50,000; 1 year)
Research Team: Dr. Pierre Blier (Principal Investigator), Dr. Natalia Jaworska, Dr. Jennifer Phillips, Ms. Katie Dinelle
A common approach for rapid intervention in cases of severe depressive symptoms has traditionally been electroconvulsive therapy (ECT) – however, a striking recent breakthrough in the field of mood disorders research has been intravenous ketamine administration. This multi-site study will compare patients’ response and remission rates with ketamine treatment versus ECT, to help inform treatment and intervention strategies. Because ketamine treatment is much less expensive and less labour-intensive to administer than ECT, the results from this study could be a boon for increasing accessibility to care through treatment alternatives for major depressive disorder.
The cholinergic system and cognitive impairments in schizophrenia
(Funded $50,000; 1 year)
Research Team: Dr. Lauri Tuominen, Dr. Synthia Guimond (Co-Principal Investigators), Dr. Jean-Paul Soucy, Dr. Robert deKemp, Dr. Gassan Massarweh, Dr. Clifford Cassidy, Dr. Jared van Snellenberg, Dr. Alain Labelle
The brain’s cholinergic system is critical for cognitive processes such as attention, working memory and learning. It has been hypothesized that decreased cholinergic neurotransmission underlies cognitive deficits in schizophrenia -- however, there has only ever been one in vivo study that examined the cholinergic system in schizophrenia. As a result, there are currently no effective drug treatments for cognitive impairments in schizophrenia. To help better inform the development of treatment to target cognitive deficits in schizophrenia patients, this study will look at cognitive impairments using advanced neuroimaging technology (combined PET-MRI).
How are brain and heart connected? Imaging of psycho-cardiac coupling in depression and atrial fibrillation
(Funded$49,619; 1 year)
Research Team: Dr. Rebecca Thornhill (Principal Investigator), Dr. Georg Northoff
Research has shown that there exists a strong brain-heart connection. Cardiac patients often show psychiatric symptoms such as anxiety and depression, for example, and psychiatric patients with major depressive disorder, bipolar disorder and anxiety disorders often show abnormalities in their heart function. While this link has been shown to exist, the reasons behind this overlap between cardiac and psychiatric disorders remains unclear. Given that the comorbidity of cardiac and psychiatric symptoms increases both symptom severity and mortality, proper diagnostic markers (i.e. biomarkers) are urgently needed. This project seeks to better understand the brain-heart connection, in order to help inform the development of biomarkers in combined psychiatric and cardiac clinical conditions.
The prevalence of chronophilic interests among adult Canadians: Development of a new online assessment method for large samples
(Funded $49,553; 1 year)
Research Team: Dr. Martin Lalumière (Principal Investigator), Enya Levaque, Dr. Michael Seto, Dr. Jonathan Gray, Dr. Skye Stephens
This study will be the first of its kind to assess chronopilias - that is, atypical sexual interests and acts associated with specific maturity categories across the lifespan – in a representative sample of Canadian adults using both direct and indirect measures. The goal of this research is to increase the scope of sexuality studies; better understand the link between paraphilias and mental disorders; and help inform new techniques to diagnose paraphilias and prevent suffering.
An examination of mechanisms that facilitate incestuous sexual behaviour by brothers and fathers
(Funded $49,893; 1 year)
Research Team: Dr. Michael Seto (Principal Investigator), Ms. Lesleigh Pullman, Dr. Jan Antfolk, Dr. Kelly Babchishin, Ms. Susan Curry, Dr. Greg Motayne
There can be serious mental and physical health costs associated with child sexual abuse, and incest victims experience greater negative consequences than victims of child abuse committed by non-relatives. Better understanding the causes of incest are vital to help with prevention, and treatment of the perpetrators. This study will build on previous research to better understand factors associated with incestuous sexual behaviour.